Cardiovascular Health – Exercise Is A Natural Treatment For Heart
The health of the heart and blood arteries is referred to as "cardiovascular health."
Obesity and its accompanying co-morbidities are on the rise in the United States and throughout the globe.
Obesity raises the risk of cardiovascular disease (CVD), type 2 diabetes (T2D), some malignancies, and mortality.
Regular physical activity provides several advantages for general health.
While losing weight and adiposity are not the significant goals of exercise, it may help mitigate the effects of obesity-related disorders such as T2D and CVD.
Several recent studies have shown that regular physical exercise is related to lower levels of inflammation, better metabolic health, a lower risk of heart failure, and better overall survival.
Exercise improves overall metabolic health and lowers the risk of developing T2D by increasing glucose tolerance, insulin sensitivity, and circulating lipid concentrations.
Physical activity may also enhance cardiovascular function by modifying the heart and vascular system.
Physical activity reduces resting heart rate, blood pressure, and atherogenic indicators while increasing physiological cardiac hypertrophy.
Exercise enhances myocardial perfusion and raises HDL cholesterol levels, relieving stress on the heart and improving cardiovascular function in healthy and ill people.
What Causes Cardiovascular Disease
The most significant cause of illness and death globally is cardiovascular disease (CVD).
Almost half of all individuals in the United States have at least one CVD risk factor (i.e., high blood pressure, high cholesterol, or smoking).
Obesity-related CVD is becoming more common.
This may happen for various reasons, one of which is that a high-fat diet or obesity can contribute to hypertension.
Sustained hypertension raises left ventricular afterload, making the left ventricle work harder, resulting in diminished myocardial function and the beginning of heart failure.
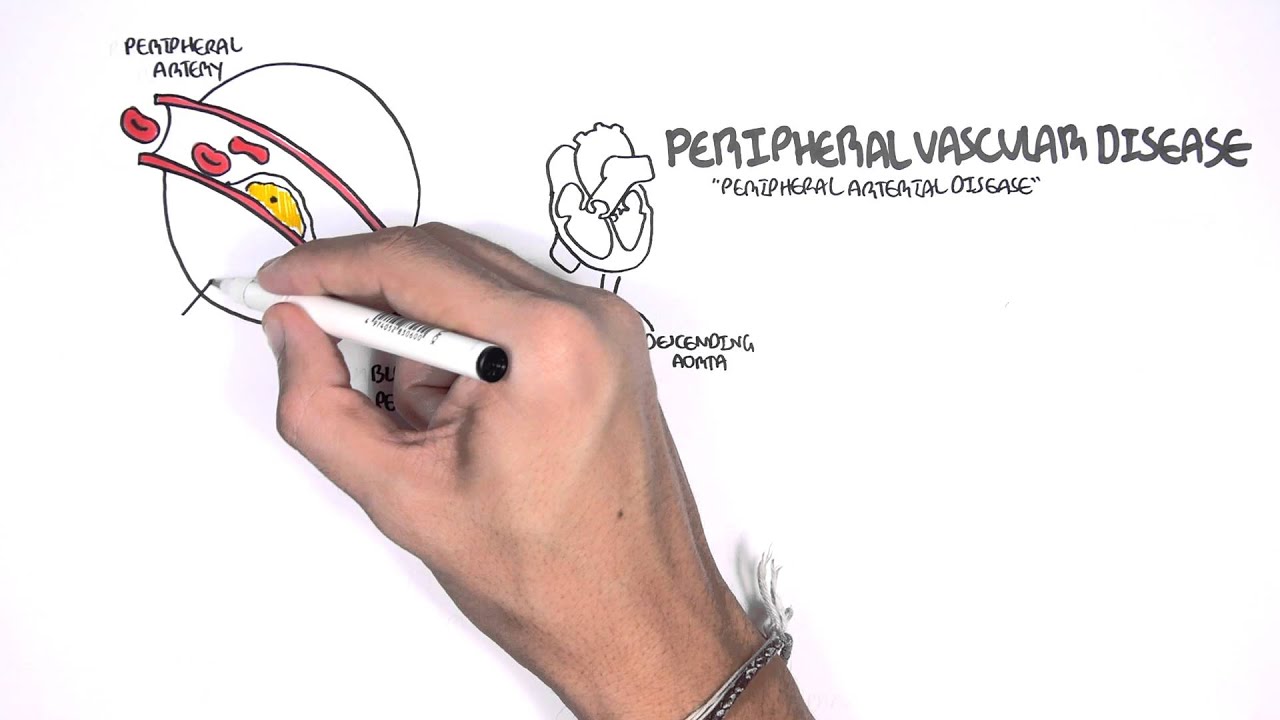
Atherosclerosis is the most frequent kind of CVD, and it develops slowly in response to chronic exposure to an unhealthy, sedentary lifestyle, including obesity.
Obesity raises circulating triglyceride and LDL cholesterol levels, causing tiny plaques to develop underneath endothelial cells on the innermost surface of artery walls.
Plaques that form cause vessel walls to thicken and harden, reducing blood flow.
Cardiovascular Disease Overview
Cardiovascular Health Exercise
One of the most important contributors to the onset and progression of cardiovascular disease is adopting a sedentary lifestyle.
Other variables, such as smoking and high blood pressure, also have a role.
Obesity and persistently low physical activity levels are two characteristics of leading a sedentary lifestyle.
Therefore, lifestyle therapies promoting physical activity and reducing obesity are appealing therapeutic techniques to address most non-congenital forms of cardiovascular disease.
Exercise Reduces Cardiovascular Related Risks
Regular physical activity has been linked to various health advantages, including reducing the progression and development of obesity, T2D, and CVD.
In several randomized clinical studies, exercise and a balanced diet have enhanced cardiovascular health in at-risk individuals.
Exercise can enhance metabolic and cardiovascular health, including glucose homeostasis and blood pressure, regardless of body weight.
Exercise leads to considerable cardiovascular and metabolic health benefits, regardless of body mass.
A 16–20 percent increase in energy expenditure (of any exercise, no diet intervention resulted in a 22.3 percent decrease in body fat mass in a one-year trial of non-obese people.
In patients who are lean, obese, or have type 2 diabetes, exercise therapies reduce the risk or severity of CVD.
Exercise Improves Cardiovascular Function In CVD Patients
According to a comprehensive analysis of 63 trials, exercise-based cardiac rehabilitation increased cardiovascular function.
Overall, exercise reduced CVD-related mortality, lowered MI risk, and improved overall quality of life.
Patients who exercised on a cycle ergometer for 60 minutes per day experienced a 29% increase in blood flow reserve and increased endothelium-dependent vasodilation.
In heart failure patients, moderate-intensity exercise-based rehabilitation improves cardiorespiratory fitness and enhances exercise endurance capacity and VO2max (12–31 percent).
WalkiAccording to one research, walking or cycling at 60–70 percent of heart rate reserve 3–5 times per week for over three years increases health and general quality of life.
Other research has looked at the effects of high-intensity exercise training on heart failure patients.
These studies show that moderate and high-intensity exercise enhances cardiovascular function, likely due to increased endothelium-dependent vasodilation and higher aerobic capacity.
Mechanism Of Exercise-Related Cardiovascular Benefits
Regular exercise improves heart health in several ways
Exercise challenges whole-body homeostasis and affects many cells, tissues, and organs in response to increased metabolic demand, including the cardiovascular system.
Exercise adapts bodily cells and tissues.
Exercise boosts aerobic respiration in adipocytes, skeletal muscle myocytes, and cardiomyocytes.
Exercise enhances oxygen supply via vasodilation and angiogenesis, preventing cardiac ischemia-reperfusion damage.
Exercise has a long-term anti-inflammatory impact that is inversely connected to CVD and obesity-related inflammation.
Myokines produced from skeletal muscle during exercise partly mediate anti-inflammatory effects and facilitate inter-tissue crosstalk for cardiovascular benefits.
- Effect On Mitochondrial Function: Many of the advantages of exercise are attributable to mitochondrial adaptations all across the body. Exercise-induced improvements in mitochondrial activity are vital in reducing the cardiovascular problems often caused by obesity. Fatty acid absorption and utilization are reduced in heart failure, which is thought to cause the heart failure-related shift toward glucose metabolism. Exercise-induced mitochondrial adaptations minimize oxidative damage caused by ischemia-reperfusion, resulting in minor heart injury. This lowers the risk of heart malfunction or mortality caused by ischemia.
- Effect On Chronic Inflammation: Inflammation is a typical response to harmful stimuli. Chronic inflammation causes obesity, T2D, and CVD. Excess nutrients cause adipocytes, hepatocytes, islet cells, and skeletal muscle cells to activate NF-B and AP-1, increase TLR4 expression, and release cytokines such as TNF-, IL-6, IL-1, and CCL2. The following inflammation is minor compared to infection or damage but lingers as a persistent reaction to obesity called "meta-inflammation." Exercise reduces inflammation long-term. Exercise reduces monocyte concentration and inhibits TNF production and other pro-inflammatory adipokines, generating an anti-inflammatory impact. Obesity-caused immunological activation is of particular significance for vascular health since TLR4 activation leads to monocyte recruitment and conversion to foam cells, promoting atherosclerosis. Exercise inhibits atherosclerosis via lowering TLRs on monocytes and macrophages, which reduces TLR4 ligands and pro-inflammatory cytokine production. Exercise reduces pro-inflammatory NT-proBNP and hsCRP in the heart, both predictors of heart failure in atherosclerosis.
- Effect Of Myokine Release on Inter-tissue Communication:Myokines produced during exercise influence organ cross-talk and improved cardiometabolic health. Over a decade ago, IL-6 was launched as the first myokine. Myonectin (MyoN) promotes fatty acid uptake in adipose tissue and protects the heart from ischemia injury. Myonectin is a glycoprotein released and belongs to the follistatin protein family. It is increased in skeletal muscle in response to exercise. Following ischemia-reperfusion, systemic treatment of Fstl1 reduced apoptosis, inflammation, and damage size. Neurons-Derived Neurotrophic Factor (NDNF) is a hypoxia-induced pro-angiogenic factor promoting endothelial cell network development via the Akt/eNOS signaling pathway. In post-MI hearts, higher NDNF levels are associated with less myocardial hypertrophy and apoptosis.
People Also Ask
Which Drink Is Best For Heart?
It's possible that drinking plain old water is the best thing you can do for your overall health, including the health of your heart.
How Do I Make My Heart Stronger?
Here are seven powerful ways you can improve your cardiovascular health.
- Your heart is a muscle, and just like any other muscle in your body, it may be strengthened via physical activity.
- Quit smoking. Quitting smoking is not an easy task.
- Lose weight. Diet and exercise alone are not enough to cause significant weight loss.
- Eat meals that are good for your heart.
- Remember to bring some chocolate.
- Don't overindulge in food
- Try to relax.
How Do I Know If My Heart Is OK?
Suppose you have a blood pressure cuff or a pulse monitor. In that case, you may assess your heart rate more precisely to determine whether or not you are in a healthy physical condition relative to your age, gender, and weight group.
The number of times your heart beats in one minute is your heart rate.
Adults should strive to have a resting heart rate between 60 and 100 beats per minute.
Conclusion
Obesity-related cardiovascular disease is on the rise, and it is often coupled with other co-morbidities such as type 2 diabetes.
Exercise decreases cardiovascular risk variables, and this reduction is independent of changes in body weight.
Exercise is also an important therapeutic option for persons suffering from cardiovascular disease.
Exercise is advantageous to cardiovascular health, but molecular mechanisms remain uncovered by its positive benefits.
More research into the molecular processes by which exercise improves cardiovascular function will develop medicines that may be used in combination with exercise regimens.
Exercise-induced myokines may be valuable targets for heart disease prevention and therapy and interventions for individuals who are unable or unwilling to exercise.